KELOID
What are keloids? How do you get them?
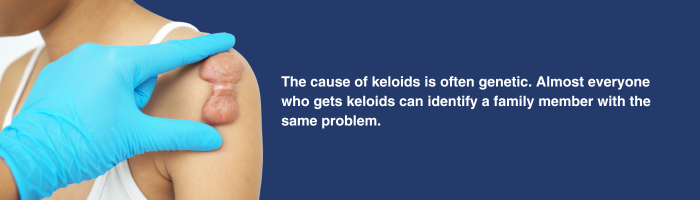
Keloids are a common problem, with the cause often being genetic. Almost everyone who gets a keloid can identify a family member with the same problem. They are difficult to live with and can also be difficult to treat. Keloids can itch, cause pain, and get infected due to buried follicles. They can also grow from the most innocuous of skin injuries like a scratch. Typically, keloids occur after cuts, surgery, trauma, and infected cysts. They will typically have a period of rapid growth which then slows down. Sometimes, keloids do not slow down and require aggressive treatment.
What do keloids look like?
Keloids have a varied appearance. They will usually enlarge, sometimes very quickly for no reason at all. Keloids can grow well beyond the original site where the problem started. They can invade and disfigure or destroy the area that is affected.
Keloids and hypertrophic scars can easily be mistaken for each other. They may look similar but they are different conditions. This will be evaluated during the office examination, with an accurate diagnosis being confirmed through pathological sample or excision.
Some characteristics of keloids could be:
- Painful
- Hard to touch
- Shiny appearance
- Raised above the skin
- Itchy
- Lumpy appearance
- Sometimes have hair growing through keloid
- Continuing to grow and spread
- New ones are red or purple
- Older scars may turn pale and flatten with time
Why remove keloids?
Keloids that are flat and painful are often found in the midline of the chest. However, they can occur on any part of the body. Keloids are caused by the overreaction of the body to injury, producing more scar tissue than is necessary. Keloids can be painful and can occur at any age. They can affect how patients are able to function in everyday life and work. The management of keloids can be complex and may need multiple modes of therapy and treatment. If left untreated, keloids of the face, neck and body can be disfiguring and affect daily life and function.
How do you treat keloids?
The treatment for keloids is typically a combination of treatment methods. Smaller keloids are treated by injection only. Most keloids that are larger will benefit from a combination of surgery and injection. Some keloids also benefit from additional radiation therapy in combination with surgery.
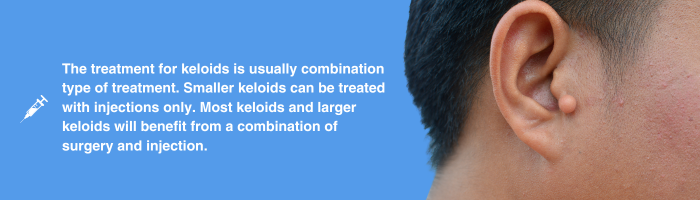
If the keloid is very small and amenable to injection, then steroid injections are the first line of therapy. However, these areas must be small, with the steroid injected directly into the keloid for it to be effective. This treatment is then repeated in 3-6 week intervals until the keloid shrinks.
Very large or bulky keloids can be reduced in size with steroid injection, but not treated completely. A better option is to remove the keloid surgically or with cryotherapy and then inject the area with steroids. The volume reduction can be performed via nonsurgical means including lasers, cryotherapy (freezing) or surgical excision. Cryotherapy involves using a special needle called cryoshape that is placed inside the keloid. Liquid nitrogen is then passed into the keloid, freezing it from within. The keloid will shrink, and then the remnant will subsequently fall off. This is then followed with the steroid injections.
Sometimes, keloids can be a recurring issue. The final line of therapy for patients who have recurrence after the steroid injections and the surgical reduction is a re-excision, followed by low-dose radiation therapy if appropriate for the area of the keloid. The benefits and risks of low-dose radiation therapy will be discussed with the patient.
Will insurance cover keloids?
Keloid removal is considered a medically necessary procedure by insurance. All insurance companies and Medicare will cover keloid removal procedures and reconstruction.